Introduction
Erectile dysfunction (ED) is often portrayed as an inevitable part of aging, a silent yet pervasive condition that robs men of confidence and intimacy. However, the story is far more complex. ED is not merely a urological inconvenience; it is a sentinel marker of vascular health, psychological well-being, and overall quality of life. In the general population, ED affects up to 50% of men over 50 years old, with prevalence increasing steadily with age. Yet, in specific groups such as military veterans, the burden of ED assumes unique contours shaped by physical illness, psychiatric comorbidity, and lived experience of service.
Veterans constitute a distinctive clinical population. Their medical history is often marked by higher rates of cardiovascular disease, post-traumatic stress disorder (PTSD), traumatic injuries, and exposure to demanding occupational stressors. These factors converge to create a multifactorial risk environment for ED, with biological and psychological determinants reinforcing one another. Unlike civilian populations, veterans may also exhibit different attitudes toward masculinity, intimacy, and help-seeking, which can influence how ED is reported and treated.
A large retrospective analysis of over 1,200 male veterans seeking treatment for ED provides fresh insight into how age, medical comorbidity, psychiatric burden, and sexual behavior intersect in this population. The findings challenge simplistic assumptions—such as “older equals worse function”—and instead reveal nuanced patterns requiring tailored management strategies. Within this framework, pharmacological interventions like sildenafil, vacuum erection devices, and psychosexual counseling occupy different niches depending on patient age and comorbidity.
Veterans as a Population at Risk: Unique Challenges
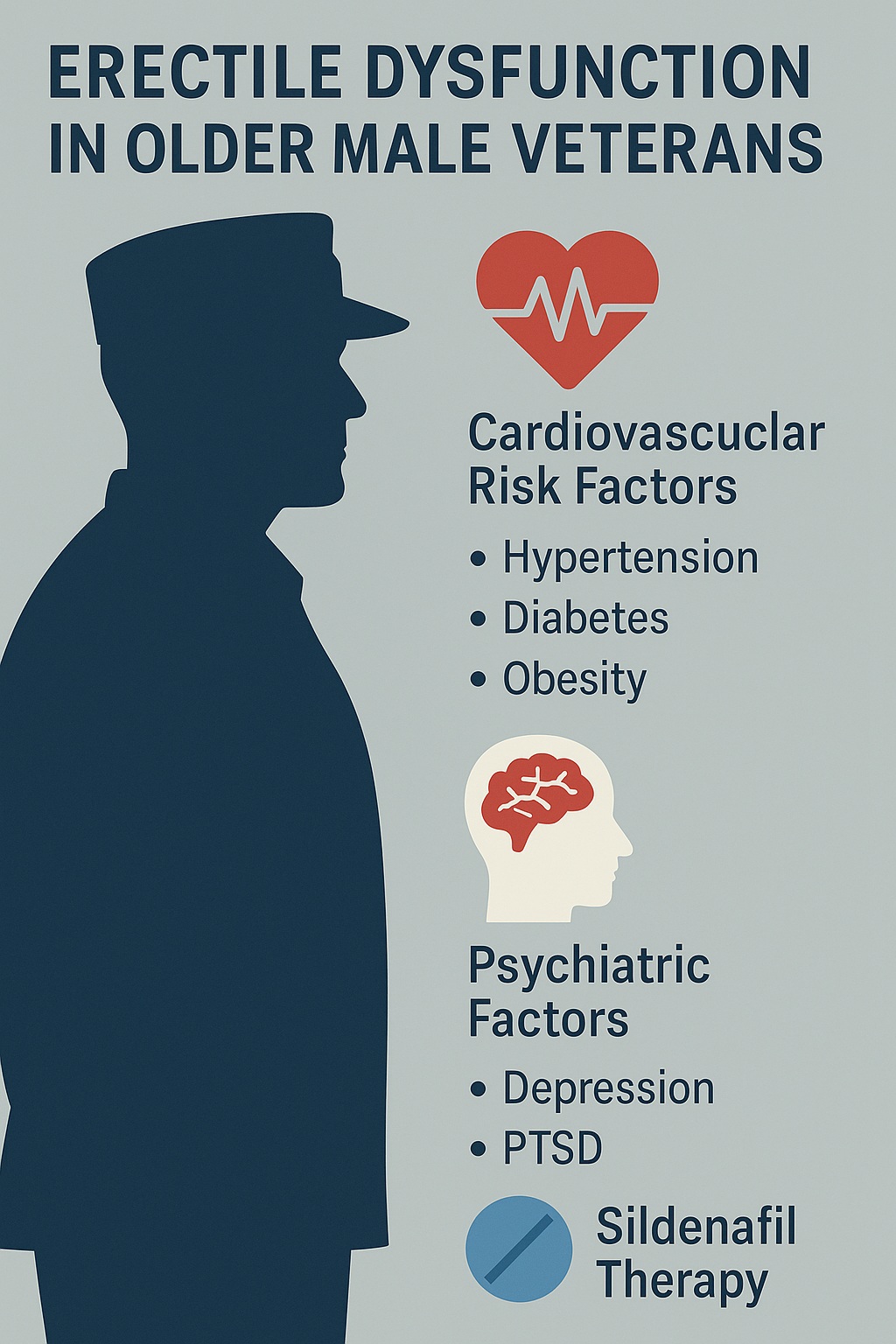
Military service imprints on health in ways both obvious and hidden. The cumulative burden of physical strain, injuries, environmental exposures, and psychological trauma translates into higher prevalence of chronic diseases among veterans compared with civilians. Cardiovascular risk factors—including hypertension, diabetes, and obesity—are especially common and directly relevant to erectile function, given the dependence of erections on vascular integrity.
ED in veterans cannot be viewed purely through the lens of penile physiology. It must be situated within a broader context of service-related injuries and psychosocial sequelae. Traumatic brain injury and spinal cord injuries, more frequent among combat-exposed veterans, may damage neural pathways critical for sexual arousal and erectile response. Likewise, long-term musculoskeletal pain and disability may limit sexual activity, not because erections are impossible but because intimacy becomes physically taxing.
Psychiatric disorders also loom large. Veterans exhibit elevated rates of depression, anxiety, substance misuse, and PTSD. These conditions, independently associated with ED, are further compounded by psychotropic medications—antidepressants, antipsychotics, benzodiazepines—that blunt libido and impair erectile physiology. Thus, the veteran population embodies a near-perfect storm: vascular, neural, psychological, and pharmacological insults converging on a single functional outcome.
Medical Determinants of ED in Older Veterans
The retrospective analysis revealed that older veterans were disproportionately affected by urological and systemic medical comorbidities. Chief among these were prostate-related conditions. Benign prostatic hyperplasia (BPH), lower urinary tract symptoms, and prior prostate cancer treatments were more common in the older cohort. These conditions not only impair urinary function but also disrupt sexual health through overlapping pelvic mechanisms.
Cardiovascular disease emerged as another dominant factor. Coronary artery disease, hypertension, diabetes mellitus, and hyperlipidemia were significantly more prevalent among older veterans with ED. Each of these conditions contributes to endothelial dysfunction, reduced nitric oxide bioavailability, and impaired penile blood flow. The overlap between vascular disease and ED is so strong that ED has been dubbed the “canary in the coal mine” for cardiovascular pathology. In veterans with established coronary disease, ED may represent both a consequence of shared risk factors and a harbinger of worsening vascular decline.
Another striking finding was the cumulative medication burden. Older veterans were more likely to be taking antihypertensives, beta-blockers, and diuretics—agents known to exacerbate ED. While life-saving, these medications inadvertently worsen erectile performance, creating therapeutic dilemmas. Clinicians must balance cardiovascular protection against quality-of-life considerations, sometimes switching to ED-friendlier alternatives such as ACE inhibitors or calcium channel blockers.
Psychiatric and Psychosocial Drivers in Middle-Aged Veterans
While older veterans carried heavier medical baggage, middle-aged veterans were more likely to present with psychiatric comorbidities. Anxiety disorders, depressive symptoms, and substance use were prominent in this group. Unlike the vascular-driven ED of their older peers, middle-aged veterans often experienced performance anxiety, relationship strain, or diminished libido linked to mental health conditions.
Tobacco use was also more prevalent among younger and middle-aged veterans, reflecting cultural patterns within military service. Nicotine-induced vasoconstriction directly impairs penile hemodynamics, while smoking accelerates atherosclerosis, amplifying long-term risk. Thus, the combination of anxiety, depressive disorders, and smoking created a unique psychosocial-vascular hybrid of ED.
Importantly, psychiatric burden also influenced treatment-seeking behavior. Veterans with depression or PTSD may be reluctant to discuss sexual problems, perceiving them as a personal failing rather than a medical condition. Stigma remains a significant barrier. When they do seek help, these veterans often require a dual approach: pharmacotherapy for ED itself and concurrent treatment of psychiatric comorbidities. Failure to address both dimensions risks frustration and dropout from care.
Sexual Behavior and Perceptions Across Age Groups
An intriguing aspect of the study was the discrepancy between objective measures of erectile function and subjective experiences of sexuality. Younger veterans reported higher levels of sexual activity, reflecting life stage and relationship dynamics. They were more likely to attempt intercourse multiple times per week, and their erectile rigidity scores were generally higher than those of older men. Yet, paradoxically, subjective distress over ED did not differ significantly across age groups.
This paradox suggests that the meaning of sexual activity changes with age. For younger men, ED threatens identity, virility, and relational intimacy, fueling anxiety. For older men, reduced activity may already be anticipated, and expectations recalibrated. As a result, older veterans, despite objectively poorer function, may report similar levels of distress as younger counterparts. This underscores the importance of contextualizing ED not only in biological terms but also in psychological and relational terms.
Another finding was that many veterans, regardless of age, had partners with their own sexual health challenges. Female partner menopause, male partner comorbidities, or relational strain influenced satisfaction. Thus, ED must be managed not in isolation but within the dyad of intimate partnership.
Treatment Modalities: From Sildenafil to Vacuum Devices
Management of ED in veterans mirrored patterns seen in the general population but with notable age-specific trends. Older veterans were more likely to be prescribed vacuum erection devices (VEDs). These non-pharmacological tools create negative pressure to draw blood into the penis, followed by application of a constriction ring to maintain rigidity. While effective, VEDs are often considered cumbersome, and adherence rates are modest.
By contrast, younger and middle-aged veterans were more likely to receive oral pharmacotherapy, particularly PDE5 inhibitors such as sildenafil. Sildenafil’s mechanism—enhancing nitric oxide–cGMP signaling—makes it particularly effective in cases where vascular and neural pathways are intact but suboptimally functioning. In veterans with performance anxiety or psychogenic overlay, sildenafil provides not only physiological support but also psychological reassurance, breaking cycles of anticipatory failure.
However, sildenafil is not a panacea. Its efficacy is reduced in veterans with severe diabetes, radical pelvic surgery, or profound neurovascular damage. Side effects—headache, flushing, nasal congestion—are generally well tolerated but may limit use in some. Importantly, sildenafil is contraindicated in veterans taking nitrates for angina, a not-uncommon scenario in this population. Alternative agents, such as intracavernosal injections or penile implants, may be required for refractory cases.
The study highlights that age stratification shapes therapy selection: younger veterans gravitate toward pills, older veterans toward devices. This reflects not only physiology but also attitudes toward convenience, spontaneity, and acceptability.
Integrating Rehabilitation and Holistic Care
Pharmacological and mechanical interventions alone are insufficient. Veterans benefit from a rehabilitation-oriented, multimodal approach. Psychosexual counseling should be integrated into routine ED management, particularly for those with psychiatric comorbidities. Cognitive-behavioral therapy can reduce performance anxiety and improve relational communication.
Lifestyle interventions are equally critical. Smoking cessation, weight management, regular exercise, and improved sleep hygiene enhance vascular health and erectile outcomes. These measures also dovetail with broader cardiovascular risk reduction, aligning sexual health with longevity.
For older veterans with multiple comorbidities, coordinated care among urologists, cardiologists, psychiatrists, and primary care physicians is essential. Addressing polypharmacy, optimizing endocrine status (including testosterone levels), and managing depression can all improve outcomes. A siloed approach risks missing interdependencies that define ED in this complex population.
Clinical Implications and Future Directions
The findings from veteran cohorts challenge simplistic age-based assumptions about ED. Older veterans are not simply “worse off”; rather, they present with a different spectrum of drivers—medical and vascular rather than psychiatric and behavioral. Recognizing this distinction allows for more precise, individualized treatment planning.
Future research should pursue longitudinal designs to track veterans across decades, clarifying causal trajectories from military service through midlife into old age. Incorporation of biomarkers—vascular imaging, hormonal assays, neurocognitive testing—may refine risk stratification. Importantly, interventional studies must evaluate not only erectile rigidity but also patient-centered outcomes such as satisfaction, intimacy, and quality of life.
Pharmacological horizons may also expand. Novel PDE5 inhibitors, soluble guanylate cyclase stimulators, and regenerative therapies (stem cell injections, platelet-rich plasma) are under investigation. Yet sildenafil remains a cornerstone, a reminder that sometimes the simplest interventions—when properly applied—carry the greatest impact.
Conclusion
Erectile dysfunction in older male veterans is not a monolithic condition but a complex interplay of biology, psychology, and social context. While older veterans predominantly present with vascular and prostate-related comorbidities, middle-aged veterans grapple with psychiatric burdens and behavioral risk factors. Younger veterans, though more active, are equally vulnerable to the distress of ED, albeit from different mechanisms.
Management must therefore be individualized. Sildenafil and other PDE5 inhibitors offer reliable benefits, especially for younger veterans with intact vasculature. Older veterans may find more utility in mechanical devices or multimodal rehabilitation strategies. Ultimately, effective care requires a holistic, patient-centered approach that honors not only the physiology of erection but also the lived reality of intimacy, identity, and resilience after service.
FAQ
1. Why are veterans at higher risk for erectile dysfunction compared to civilians?
Veterans face higher rates of cardiovascular disease, PTSD, injuries, and psychiatric disorders, all of which contribute to ED. Medications for these conditions may also impair sexual function.
2. How effective is sildenafil for veterans with ED?
Sildenafil is effective in about two-thirds of veterans, particularly those with mild to moderate vascular compromise. Its benefit is reduced in cases of severe neurovascular injury or when contraindicated by nitrate therapy.
3. Do older and younger veterans respond differently to treatment?
Yes. Older veterans are more often managed with vacuum devices due to comorbidities and medication interactions, while younger veterans are more likely to use oral PDE5 inhibitors such as sildenafil.
4. Can erectile dysfunction in veterans be prevented?
While not always preventable, risk can be reduced by managing cardiovascular disease, quitting smoking, addressing psychiatric conditions, and using early interventions such as rehabilitation and PDE5 inhibitors.
References
- Cosgrove DJ, Gordon Z, Bernie JE, et al. Erectile dysfunction in combat veterans. Sex Med Rev. 2014;2(2):87–93.
- Incrocci L, Slagter C, Hop WC, van der Poel HG. Sildenafil use and sexual function after radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2006;66(2):439–444.
- Cosgrove DJ, Gordon Z, Bernie JE, et al. Sexual dysfunction in combat veterans with post-traumatic stress disorder. Urology. 2002;60(5):881–884.
- DeBerardis D, Marini S, Fornaro M, et al. Erectile dysfunction among male veterans with psychiatric disorders: A neglected clinical concern. Psychiatry Investig. 2018;15(2):123–129.
- Incrocci L, Wortel RC, Alemayehu WG, Heemsbergen WD, Heijmen BJ, Pos FJ. Dose to penile bulb is not associated with erectile dysfunction 18 months post radiotherapy: Secondary analysis of a randomized trial. Clin Transl Radiat Oncol. 2018;13:1–6.
- Cosgrove DJ, Carpenter MJ, Chengappa KNR. The interaction of smoking, psychiatric illness, and sexual dysfunction. Curr Sex Health Rep. 2015;7:124–131.
- Goldstein I, Mulhall JP, Bushmakin AG, Cappelleri JC, Hvidsten K. The erection hardness score and its relationship to successful sexual intercourse. J Sex Med. 2008;5(9):2374–2380.
- Cosgrove DJ, Gordon Z, Bernie JE, et al. Clinical characteristics of older male military veterans seeking treatment for erectile dysfunction. Int Psychogeriatr. 2011;23(1):96–104.